by Tanya Keam | Jan 31, 2024 | Acupuncture, chinese herbal medicine, Chinese medicine, Client information, Fertility, Gynaecological, Menstrual cycle, PCOS, Period pain, PMS, Polycystic Ovarian Syndrome, pregnancy, Self care, Sunshine coast
Polycystic Ovarian Syndrome
Polycystic ovary syndrome (PCOS) is a hormonal problem that happens during the reproductive years. If you have PCOS, you may not have periods very often or your cycle is rarely a monthly cycle. Or you may have periods that last many days (1).
PCOS is classed as a hormonal and metabolic health imbalance affecting approximately 1 in 10 women. The male hormones androgens are higher in women with PCOS, as well as problems with insulin. Insulin is a peptide hormone secreted by cells of the pancreas to help maintain normal blood glucose levels, regulating carbohydrate, lipid and protein metabolism and promoting cell division and growth through its mitogenic effects (2). When insulin becomes resistant, that’s when disharmony with weight and hormonal changes can occur in women, thus having an impact on their reproduction.
What are the symptoms of Polycystic Ovarian syndrome?
- Irregular or no periods
- Excessive hair growth on the face or body
- Hair loss
- Skin conditions such as acne or excessive skin tags
- Difficulty falling pregnant due to irregular ovulation
- Difficulty losing weight and/or weight around the waist
- Mood changes and/or specifically anxiety or depression
Possible causes for Polycystic Ovarian syndrome
Genetics may play a role in PCOS, with up to a third of women having a female relative with PCOS or similar without being diagnosed. However lifestyle, diet and environmental factors show to be contributing factors also.
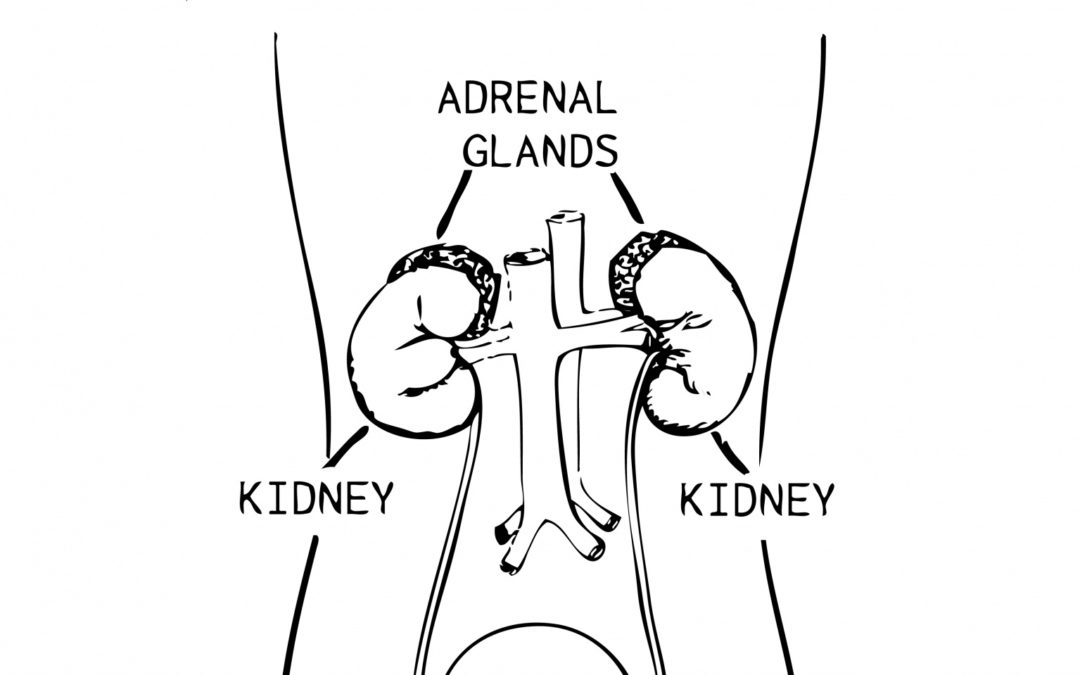
It is important to note that females can experience irregular periods without any of the other above symptoms. This is classed as polcystic ovaries (PCO); when you have multiple “cysts” on the ovaries. They aren’t actually cysts, they’re eggs that haven’t developed properly. It might occur after hormonal conceptive use in the reproductive years that confuse the body, and/or lifestyle or environmental factors. Insulin and weight are usually not of concern with PCO. The hypothalamic-pituitary-adrenal axis (HPA), describes the interaction between the hypothalamus, pituitary gland, and adrenal glands. The hypothalamus and pituitary gland are located just above the brainstem, while the adrenal glands are found on top of the kidneys (3). The HPA can receive the wrong signals resulting in eggs that haven’t developed properly (cysts), thus causing lack of ovulation and periods (4). Distinguishing between PCOS and PCO is important.
What can help Polycystic Ovarian syndrome?
PCOS treatment is mainly focussed on symptom management by reducing additional metabolic risk factors like heart disease and diabetes. Other ways can include:
- Regular exercise – managing potential weight gain and maintaining a healthy cardiovascular system
- Dietary changes – as PCOS has a somewhat inflammatory component, reducing inflammation via appropriate foods (a Mediterranean diet). Moderating carbohydrate intake in a similar way to balancing diabetes (insulin imbalances). Minimising exposure to foods that contain hormones that have been purposefully added to increase production – animal products usually.
- Acupuncture – can help with pain associated with PCOS and help regulate the nervous system which in turn has an impact on hormones
- Managing stress – stress impacts any health condition. Learning to manage life’s stressors is vital for general health and well being. Low stress also equals low cortisol release (the stress hormone). High cortisol leads to weight gain thus impacting the metabolic pathways exasperating PCOS
- Reducing exposure to hormone disrupting chemicals – did you know that IVF clinics do not allow perfumes/deodorants into their clinics as research has found that they can disrupt the endocrine system. In the armpit for example, products get directly absorbed into the lymphatic system. Going as natural as possible with skin care, body products and cleaning products will surely benefit
What does research say about Chinese medicine and Acupuncture for PCOS?
A study done in 2018 on the prevalence of diabetes mellitus, obesity, lipid metabolism disorders, and major depression was recorded as common symptoms for PCOS enrolled patients. Multiple common Chinese herbal formulas were included in the study based on the patients symptoms such as period pain, abdominal pain, constipation and uterine contractions.
The present findings revealed that patients with PCOS had a relatively high tendency to consult TCM practitioners (89.22%) due to Western medicine not having a treatment protocol directly. Among these prescription chinese herbal medicines (CHM) trialled showed hepatoprotective effects, as well as beneficial effects in treatment of hyperglycemia, insulin intolerance, dyslipidemia, and anovulation. These findings indicate that Chinese herbal medicine might serve as a potentially effective therapeutic option for PCOS (5).
Another study showed that following transfer of fresh or frozen-thawed embryos available from the same stimulated IVF cycle, 47 patients got clinical pregnant and 43 of them achieved live birth with the use of CHM. Among which, 32 patients achieved term delivery in the CHM group. In the non-CHM group, 27 patients got clinical pregnant and 22 of them achieved live birth, among which, 14 patients achieved term delivery (6).
The NHMRC Centre for Research Excellence in PCOS undertaken at the Sydney Western University, has already completed a systematic review, and a qualitative study on acupuncture for weight loss in PCOS, with feasibility testing now in sight for a clinical trial. The clinical trial will explore the role of traditional acupuncture as an adjunct to lifestyle interventions for weight loss in PCOS. “Weight loss improves many of the features of PCOS and can reduce the burden of chronic disease from diabetes and heart disease.” (7).
 Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Polycystic Ovarian Syndrome or Polycystic ovaries, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support your gynaecological health.
Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Polycystic Ovarian Syndrome or Polycystic ovaries, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support your gynaecological health.
You can see Tanya’s training here, call us here, or book online here.
References:
- https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
- Wilcox. G. 2005. Insulin and Insulin resistance. National Library of medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1204764/
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009 Jul;5(7):374-81. doi: 10.1038/nrendo.2009.106. Epub 2009 Jun 2. PMID: 19488073. https://neuroscientificallychallenged.com/posts/what-is-the-hpa-axis
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009 Jul;5(7):374-81. doi: 10.1038/nrendo.2009.106. Epub 2009 Jun 2. PMID: 19488073. https://neuroscientificallychallenged.com/posts/what-is-the-hpa-axis
- Liao, Wan-ting, Chiang. Jen-huai, Li Chia-lung, Lee Ling-Tsung, Su Cheng-chiung, Yen Hung-rong. 2018 J Clin Med. 2018 Jul; 7(7): 179. Journal of Clinical Medicine. Investigation on the Use of Traditional Chinese Medicine for Polycystic Ovary Syndrome in a Nationwide Prescription Database in Taiwan. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6069244/
- 6. P, Xiaoming. Gu, Yinger. Z Xian. W, Fangfang. S, Biwei. C, Long. W, fangfang. Q, fan. Integrative Medicine research Volume 11, Issue 1, March 2022, 1007752022. Chinese herbal medicine (Bu-Shen-Tian-Jing Formula) for outcomes of IVF in Chinese patients with polycystic ovary syndrome: A retrospective cohort study. https://www.sciencedirect.com/science/article/pii/S2213422021000627
- NICM Health Research Institute: https://westernsydney.edu.au/nicmhri/news/trial_to_explore_acupuncture_for_weight_loss_in_pcos

by Tanya Keam | Jan 24, 2024 | Acupuncture, Anxiety, Chinese medicine, Client information, Digestive health, Emotions, Herbal remedies, Irritable bowel syndrome, Loose stools, Nambour, Nutrition, Stress, Sunshine coast
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a common disorder that affects the stomach and intestines, also called the gastrointestinal tract. Symptoms include abdominal pain, bloating, cramping, gas, and diarrhoea or constipation, or both.
Only a small number of people experiencing IBS have severe symptoms, while others experience mild pain and alternation of bowel habits. So how are your insides? Worried about where the next toilet will be? Your digestion is switching from diarrhoea to constipation and you’ve tried dairy free, gluten free or the low-FODMAP diet?
Sometimes people can visit their medical physician with symptoms and either be dismissed or referred to a gastroenterologist. Sometimes people can get a parasite or gastroenteritis (infection/inflammation in the gut) from eating contaminating food/water from traveling overseas and then end up with IBS symptoms long term.
To date, the pathophysiology of IBS is still not completely understood. However, specialists are now more accepting of IBS signs and symptoms being a functional disorder with both physiological and psychosocial factors, despite x-rays, lab tests or biopsies being clear.
What might a specialist first exclude before diagnosing Irritable Bowel Syndrome?
Due to many digestive conditions having similar signs and symptoms, a specialist must first rule out other conditions such as:
- Small-bowel bacterial overgrowth
- Lactose intolerance
- Eating disorder
- Inflammatory bowel disease
- Autoimmune disease
- Coeliac disease or celiac sensitivity
- Parasites
- Infection
- Laxative use
- Microscopic colitis
- Pharmaceutical side effects
- Gastritis or Enteritis
A patient may undergo blood tests, stools tests, physical examination, colonoscopy, ultrasound or sigmoidoscopy tests and a physician will also exclude any of the above causes (1). If tests come back clear and no other gastrointestinal diseases are determined, then IBS is considered (2).
How is Irritable bowel syndrome treated ?
Doctors may treat IBS by recommending changes in what you eat and other lifestyle changes, medicines, probiotics, and mental health therapies (3).
Also:
- Increasing fibre to improve constipation
- Decreasing gas producing foods
- Following a FODMAP photocol or other dietary protocol that improves symptoms
- Mental health support
- Stress management
- Getting enough sleep
- Increasing exercise
- Drug therapy for the dominant symptoms
What does research say about other therapies such as Chinese medicine, Acupuncture and behavioural therapy?
A review of mind/body approaches to irritable bowel syndrome has suggested that alternate strategies targeting mechanisms other than thought content change might be helpful, specifically mindfulness and acceptance-based approaches (4).
Best practices in treating IBS support the idea that patients should be referred for behavioural therapy early, not just when patients have failed everything else. Ideally, consultation with a gastrointestinal psychologist would be incorporated very early into the treatment plan so that collaboration can occur between the patient, psychologist, gastroenterologist, and possibly a dietitian. IBS is a multifactorial disorder, and the field of gastroenterology is moving toward additional in-clinic assessments of mood to more comprehensively aid patients in the management of complexities associated with IBS (5).
A 2015 Australian randomised-controlled trial showed that Chinese herbal medicine may be an effective treatment in relieving IBS. The double-blinded trial was for constipation-type IBS, and it found that Chinese herbal medicine reduced symptoms, increased bowel satisfaction and stool consistency, reduced straining and hard lumpy stools, compared with placebo (6). The study also showed how quickly symptoms can improve with symptoms improving by week 8 of the trial and the herbs being well tolerated by participants.
Other research suggested by The World Journal of Gastroenterology of a meta-analysis of 6 randomised controlled trials in 2014. The review found that acupuncture clearly leads to control of IBS symptoms which is both statistically characteristic and statistically significant (7).
Moxibustion (moxa) is a technique to burn mugwort on or close to a patients skin with or without acupuncture stimulation. It is used to help relieve pain, discomfort, to encourage blood flood and alleviate other symptoms according to Chinese medicine diagnosis. A review of 20 randomised-controlled trials of managing IBS showed moxa may provide benefit to IBS patients, however further research is needed (8).
How does Chinese medicine and Acupuncture help Irritable Bowel Syndrome?
Publications of the interactions between traditional Chinese medicine and the gastrointestinal system from the years 2004 to 2021 has been widely studied, with the number of papers rapidly increasing since 2018 (9).
One of the branches of Traditional Chinese Medicine is Acupuncture, which is used to stimulate documented acupuncture points to relieve pain, treat internal organ problems, reflect on disease conditions and activate the self healing ability to keep people well.
The Acupuncturist will talk with the patient about signs and symptoms and other lifestyle or dietary factors that may be contributing to the problem. Sometimes acupuncture alone can regulate the digestive system, other times herbal medicine is prescribed alongside depending on predominant symptoms such as constipation or diarrhoea. Other symptoms are taken into account for the patients individual pattern when herbs are given.
Educating patients about lifestyle factors for managing stress is also important. We will work closely with the patient to improve their diet, reduce foods that may be contributing to IBS or other gastrointestinal problems.
 Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Irritable Bowel Syndrom, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support you to feel better.
Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Irritable Bowel Syndrom, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support you to feel better.
You can see Tanya’s training here, call us here, or book online here.
References
1. Mayo Clinic (2018). “Irritable Bowel Syndrome”. Available at: https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
2. Harvard Health Publishing (2018). ‘The gut-brain connection.’ Available at: https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection
3. National Institute of Diabetes and Digestive and Kidney Diseases (2024). ‘Treatment of Irritable Bowel Syndrome’. Available at: https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/treatment
4. Sebastián Sanchez B, Gil Roales-Nieto J, Ferreira NB, Gil Luciano B, Sebastián Domingo JJ. New psychological therapies for irritable bowel syndrome: mindfulness, acceptance and commitment therapy (ACT) Rev Esp Enferm Dig. 2017;109(9):648–657.
5. Riehl, M. (2018). ‘The Emerging Role of Brain-Gut Therapies for Irritable Bowel Syndrome.’ Gastroenterology & Hepatology14(7), 436-438.
6. Bensoussan, A., Kellow, J., Bourchier, S., Fahey, P., Shim, L., Malcolm, A. & Boyce (2015). ‘Efficacy of a Chinese Herbal Medicine in Providing Adequate Relief of Constipation-predominant Irritable Bowel Syndrome: A Randomized Controlled Trial’. Clinical Gastroenterology and Hepatology, 13(11), Pages 1946-1954.
7. Chao, C. & Zhang, S. (2014). ‘Effectiveness of acupuncture to treat irritable bowel syndrome: a meta-analysis.’ World Journal of Gastroenterology, 20(7), Available at: https://doi.org/10.3748/wjg.v20.i7.1871.
8. Park, J., Lee, B. & Lee, H. (2013). ‘Moxibustion in the management of irritable bowel syndrome: systematic review and meta-analysis’. BMC Complementary and Alternative Medicine, 13. Available at: https://bmccomplementalternmed.biomedcentral.com/articles/10.1186/1472-6882-13-247.
9. Yang, S. Hao, S. Wang, Q. Lou, Y. Jia, L. Chen,D. (2022). The interactions between traditional Chinese medicine and gut microbiota : Global research status trends. National Library of Medicine, 12: 1005730. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9510645/
Other articles:
1. Sebastián Sanchez B, Gil Roales-Nieto J, Ferreira NB, Gil Luciano B, Sebastián Domingo JJ. New psychological therapies for irritable bowel syndrome: mindfulness, acceptance and commitment therapy (ACT) Rev Esp Enferm Dig. 2017;109(9):648–657.
2. Thakur ER, Shapiro J, Chan J, et al. A systematic review of the effectiveness of psychological treatments for IBS in gastroenterology settings: promising but in need of further study [published online May 10, 2018] Dig Dis Sci. doi:10.1007/s10620-018 5095-3.
3. Keefer L, Palsson OS, Pandolfino JE. Best practice update: incorporating psychogastroenterology into management of digestive disorders. Gastroenterology. 2018;154(5):1249–1257.

by Tanya Keam | Jan 10, 2024 | Acupuncture, Bloating, Chinese medicine, Client information, Emotions, fertility acupuncture, Gynaecological, Herbal remedies, Hormones, Menstrual cycle, Nambour, Period pain, PMS, Premenstrual Dysmorphic Disorder, Self care, Stress, Sunshine coast, Womens health
Chinese Medicine for Premenstrual Dysmorphic Disorder
Premenstrual Dysmorphic Disorder (PMDD) is a health concern that is similar to premenstrual syndrome (PMS) but is more serious. PMDD causes severe moodiness such as feeling irritable, crying a lot, depression, anger outbursts or anxiety in the week or two before the period starts. Other symptoms may include fatigue, weight gain, restless sleep, breast tenderness, digestion changes, trouble focussing, binge eating, feeling out of control and suicidal thoughts.
About 80% of women report at least mild premenstrual symptoms, 20%–50% report moderate-to-severe premenstrual symptoms, and about 5% report severe symptoms for several days with impairment of functioning. The 5% of women with the severest premenstrual symptoms and impairment of social and role functioning often meet the diagnostic criteria for premenstrual dysphoric disorder (PMDD) (1).
Risk factors may include:
- A family history of PMS or PMDD
- Women with a personal or family history of depression, postpartum depression, or other mood disorders
- Cigarette smoking (2)
How is PMDD diagnosed?
Premenstrual Dysmorphic Disorder (PMDD) is typically diagnosed by a healthcare provider after performing a physical examination and speaking to the patient about signs and symptoms. Researchers do not know for sure what causes PMDD or PMS, however hormonal changes in the menstrual cycle each month may play a role due to the brain chemical called serotonin levels changing throughout the cycle.
Healthcare providers may also ask patients to keep track of symptoms over several menstrual cycles, or order tests to check certain things related to hormones.
What are the treatment options for PMDD?
Treatment for Premenstrual Dysmorphic Disorder (PMDD) typically involves a combination of lifestyle changes and medications. Medications used to treat PMDD include antidepressants, hormonal control pills/medications, or non-steroidal anti-inflammatory drugs. In some instances, gonadotropin releasing hormones may be given.
Natural approaches for Premenstrual Dysmorphic Disorder (PMDD) can include regular exercise and nutritional changes individualised to the patient to support serotonin, and lifestyle modifications such as sticking to a daily routine, practicing meditation and taking care of oneself, recognising emotions and managing stressful situations. Other natural remedies that have been used to treat symptoms associated with PMDD include acupuncture and herbal medicine.. Traditional Chinese medicinal herbs can be given to patients the week or two before their period is due to ease symptoms. This can be a good alternative to pharmaceuticals.
It’s important to remember than it’s normal for women and young girls to experience fluctuations in energy levels, mood or food cravings in different stages of their menstrual cycle. Iron levels for example drop once the uterus lining has shed, so it’s normal to feel lower energy before or on your period. Women live on a 28 day cycle and can sometimes even sync with the moon cycles. Whereas, men live on a 24 hour one! However when signs and symptoms are really affecting your quality of life, then it’s important to seek help.
 Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Chinese Medicine Premenstrual Dysmorphic Disorder treatment specifically, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support you to feel better.
Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Chinese Medicine Premenstrual Dysmorphic Disorder treatment specifically, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support you to feel better.
You can see Tanya’s training here, call us here, or book online here.
References:
- Pearlstein, T., Steiner, M. (2008). Premenstrual dysphoric disorder: burden of illness and treatment update. Journal of Psychiatry & Neuroscience; 33(4): 291–301.
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/premenstrual-dysphoric-disorder-pmdd

by Tanya Keam | May 10, 2023 | Acupuncture, Chinese medicine, Client information, Health practitioner, Jaw pain, Mental health, Muscle pain, Nambour, Private health, Rehabilitation, Sleep, Stress, Sunshine coast, TMJ, Wellness
Acupuncture for TMJ
What is TMJ?
TMJ stands for Temporo-Mandibular Joint. The TMJ is the joint that connects the jaw to the skull. These joints are involved in eating, facial movements and speech. Let’s get into how Acupuncture for TMJ pain can be helpful.
What is TMJ pain?
Pain that can feel grinding in the jaw, that if left untreated can lead to inability to chew properly, ear pain, migraine, headache, lack of sleep, tooth pain, lockjaw, dizziness, anxiety and joint noises such as cracking or popping of the jaw.
What are the symptoms you might experience from TMJ pain?
- Inability to chew food properly
- Ear pain or ear ache
- Insomnia
- Tooth ache
- Locked jaw
- Headache
- Migraine
- Mood dosorders
- Neck pain
- Dizziness
- Vertigo
How can TMJ be diagnosed?
Diagnostic tests may include:
- Xray
- MRI
- CT scan
- Physical exam by a general physician, physical therapist or other allied health professional if you are presenting with persistent jaw pain
Available treatment options for TMJ pain
- Exercises to relax or strengthen the muscles of the jaw
- Dental splints to reduce tooth grinding at night
- Dental alignment
- Stress management
- Soft tissue release to relax muscle tension in the jaw
- Diet changes such as increasing omega’s to reduce systemic inflammation such as arthritis, autoimmune or connective tissue conditions
- Pharmaceutical pain relief
- Herbal medicine
- Acupuncture
- Physical therapy
By the time a person seeks treatment, TMJ is often at its chronic stage so it does take time to treat it and using more than one type of approach would give a person a better outcome.
For example: managing stress so that a person does not grind their teeth at night thus reducing the need for a dental splint, improving diet to align with low to no inflammation in the body and seeking treatment from a qualified therapist to assist soft tissue release such as having acupuncture or having dental procedures to correct jaw and tooth alignment.
Acupuncture for TMJ:
Acupuncture therapy has been around for centuries and is often known to be able to treatment painful conditions. Aside from dental causes of TMJ, the majority of cases can be seen as a deep route of underling stress which therefore causes tension on the neck, jaw and temporal muscles of the skull. Exacerbated tension leads to exacerbated pain. The added benefits of chinese herbal medicines, diet and lifestyle advice alongside the acupuncture therapy, people can have lasting results in treating TMJ.
Current research findings for Acupuncture for TMJ:
- Acupuncture to have a positive effect in the treatment of pain associated with TMJ compared to the control groups (3).
- A 2010 study showed acupuncture treatment of TMJ achieved immediate effect in pain and showed ongoing positive effects after a treatment regime over 8 – 10 weeks of treatment (1).
- A 2012 study showed pain intensity was less in the trigger point acupuncture group than in the sham (fake acupuncture) treatment group, pain intensity decreased significantly between pretreatment and after 5 weeks, and trigger point acupuncture therapy may be more effective for chronic TMJ myofascial pain (2).
- A 2014 study showed laser acupuncture therapy improves the symptoms of treatment-resistant TMD. Further studies with a more appropriate designs specific for laser acupuncture are needed (5), however a review of acupuncture randomised control trials (3) found acupuncture showed promising results in the management of TMJ symptoms (4).
If you are suffering from TMJ pain please contact us today to discuss how we can help you at our Nambour Acupuncture clinic in the Sunshine Coast hinterland.
Hi, I’m T anya, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
anya, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
References :
- Acupuncture for Treating Temporomandibular Disorder: Retrospective Study on Safety and Efficacy: Garty Adriel, Maimon Yair, Miller Udi; Acupunct Meridian Stud 2010
- Effects of trigger point acupuncture treatment on temporomandibular disorders: a preliminary randomized clinical trial: Kazunori Itoh, Sayo Asai, Hideaki Ohyabu, Kenji Imai, Hiroshi Kitakoji; Epub 2012
- Acupuncture therapy in the management of the clinical outcomes for temporomandibular disorders A PRISMA-compliant meta-analysis: Jun-Yi Wu, MD,Chao Zhang, MD, Yang-Peng Xu, MM, Ya-Yu Yu, MD,Le Peng, PhD, Wei-Dong Leng, PhD,Yu-Ming Niu, PhD, and Mo-Hong Deng, PhD
- Acupuncture for Temporomandibular Disorders: A Systematic Review: Seung-Hun Cho KMD PhD, Wei-Wan Whang KMD PhD.
- Clinical effectiveness of laser acupuncture in the treatment of temporomandibular joint disorder: Yu-Feng Huang, Jung-Chih Lin, Hui-Wen Yang, Yu-Hsien Lee, Chuan-Hang Yu; Epub 2014
- https://www.mayoclinic.org/diseases-conditions/tmj/symptoms-causes/syc-20350941

by Tanya Keam | May 2, 2023 | Acupuncture, Autoimmune, Bloating, Chinese medicine, Chronic fatigue, Client information, Digestive health, Health practitioner, Herbal remedies, IBS, Immune system, Inflammation, Loose stools, Nambour, Nourishing, Seasonal living, Sunshine coast
Digestive health in Chinese medicine is determined by the digestive symptoms we experience. The way food is prepared and cooked affects how we absorb nutrients. Our energy level, mood, body shape and muscle mass, flavour cravings, gyneocological problems and bowel movements tell us important information. Research is now suggesting a link between the gut-brain connection with conditions like Irritable Bowel Syndrome (IBS) (1) and the effects of our mental health and stress levels impacting our gut health. From a Chinese medicine point of view the way humans can overthink and worry in the mind, directly affects the digestion. Science is just now catching up with digestive health in Chinese medicine.
In Chinese medicine, a lot of emphasis is on the energetics of the spleen organ. What does the spleen do? Its job is to digest food, coagulate blood and metabolise fluid in the body. In other words, transform food and water into energy and then transport that energy around the body to make everything our body is made up of such as blood cells and muscle.
Because our core body temperate ranges from 35.9 to 37.2, the spleen does a much better job when cooked foods are eaten. Like our tummy is a nice warm cauldron. Having an icy cold smoothie, cold breakfast and cold water throughout the day make the spleen work harder by first using energy to warm up whats been ingested, then ‘transform and transport’. Going from a 19 degree fridge temperate (or even colder if you’re eating something frozen, to a 36.5 degree stomach temperature!) So its doing double the work! Symptoms that can arise are fatigue, bloating, excessive sweet cravings, soft and/or loose stools, poor muscle tone and deficiency of minerals and nutrients due to poor absorption.
It’s not to say every meal we have needs to be cooked. But a warm cooked breakfast such as eggs or oats, starts your day off well by keeping you fuller for longer (protein makes you feel fuller so daily eggs are a good option). Salads and raw fruit is still important to consume for vitamins and minerals but ease off on them in the cooler months, or have the salad at room temperature.
Cauldrons of soups, pots of fragrant teas, bowls of steaming rice and slow cooks stews are your best friend in the cooler months because no vitamins or minerals are lost in the cooking methods (like when steaming or blanching vegetables). Instead, all of the nutrients stay in the liquid. Warm meals keep us well and energised.
For people who cannot stomach food in the morning, this is due to the stress hormone cortisol being too high. Adrenaline kicks in when you wake up to get you going for the day because Cortisol is highest first thing in the morning. Often reaching for a coffee on an empty stomach stimulates adrenaline further and people live in this cycle of cortisol – adrenaline. If you have a job where getting up at 3.30am is your day, then you’re not going to be hungry because you’re body is suppose to be still asleep, but come 6-7am your stomach should be telling you to eat something by then. If you really do enjoy a morning coffee, aim for mid morning and have food with it so the caffeine isn’t triggering adrenaline and cortisol.
Ideally, waking up to hydrate with room temperature to warm water, then eat a warm breakfast between 7-9am is best for our digestive health in Chinese medicine theory. The spleen energy kicks in from 9-11am to do its T & T function. With daily exercise, daily bowel movements should be well formed and feel complete. If you need to wipe your bottom a lot or theres quite a lot of smell or mess in the toilet are you flush – your spleen is under-fuctioning like there is a “stickiness” in your stools. In Chinese medicine we call this dampness. Acupuncture and herbal medicine can quickly harmonise this. On the other hand if you’re bowels are irregular or sluggish then the body is absorbing waste back into the body – this can lead to liver problems and further bowel problems. Research has also shown that the warm therapeutic effect of moxibustion (burning compressed mugwort on or near a person’s skin) to help alleviate various conditions involving pain and discomfort, including IBS, showed moxibustion may also provide a benefit to IBS patients in 20 randomised-controlled trial results (2).
If you are suffering from digestive symptoms mentioned above or you believe you have poor digestion, have been diagnosed with inflammatory bowel, IBS or you’re aware stress and emotions are upsetting your stomach, please contact us today to discuss how we can help your digestive health at our Nambour Acupuncture clinic in the Sunshine Coast hinterland.
Hi, I’m T anya, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
anya, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
References:
- Harvard Health Publishing (2018). ‘The gut-brain: connection. At: ’https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6111498/
- Mayo Clinic (2018). “Irritable Bowel Syndrome”. At: https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
- https://bmccomplementmedtherapies.biomedcentral.com/articles/10.1186/1472-6882-13-247#Sec7

by Tanya Keam | Aug 30, 2022 | Acupuncture, Autoimmune, Chinese medicine, Client information, Exercise, Immune Support, Immune system, Inflammation, Joint pain, Nambour, Nutrition, Pain, Stress, Sunshine coast
Acupuncture for Inflammation is showing positive results in research. Inflammation refers to your body’s process of fighting against things that harm it, like infections, injuries, and toxins, in an attempt to heal itself. When something damages the cells, your body releases chemicals that trigger a response from your immune system.
Chronic inflammation can cause autoimmune disorders, such as Lupus or Chron’s, where your body attacks healthy tissue. Exposure to toxins, like pollution or industrial chemicals. Untreated acute inflammation, such as from an infection or injury.
Other factors that contribute significantly to inflammation is poor diet and stress.
What about stress?
- Working too much, over doing it
- Poor diet
- Lack of exercise
- Environmental factors
- Emotional distress
- Not taking care of yourself
- Injury, trauma – sometimes inflammation is a good thing when there’s been trauma to the body. However its important to quickly reduce the inflammation so the body can heal and get well
Try to avoid these “foods” when grocery shopping:
- Refined carbohydrates, such as white bread and pastries
- Hot chips and other fried foods (often fried in canola oil which is GMO)
- Margarine
- Soft drinks and other sugar-sweetened beverages (including some alcoholic drinks)
- Red meat and processed meat (hot dogs, sausages)
- Corn syrup
- Packaged foods with ingredient and numbers on the ingredients list you don’t understand
- Drive-through foods
Other foods that may contribute to inflammation in the body for some people may include:
- Gluten (proteins trigger the immune system to jump into action, causing inflammation). This inflammation can affect the body’s organs and soft tissue. However sometimes, its the pesticides, herbicides or other chemicals used in the processing of certain grains which can cause gluten sensitivity.
- Dairy
- Soy
- Corn
- White sugar
An anti-inflammatory diet is rich in good oils, fats, omega’s and antioxidants…
- Olive oil, flaxseed oil
- Green leafy vegetables (such as spinach, kale, and collards)
- Nuts
- Tumeric, ginger
- Fatty fish (like salmon, mackerel, tuna and sardines)
- Fruits (such as avocado, strawberries, blueberries, cherries, goji berries, pineapple, papaya)
- Raw unprocessed honey
- Coconut
- Tomato
- Bone broth
- Ghee
- A rainbow of fruits and vegetables
Try to eat as organic and local as possible. In season fruits and vegetables are also important. Certified organic can be expensive so if you cant source it, make sure you thoroughly wash your food. Or better yet start a little vegie garden and grow what you can at home.
How can Chinese medicines and Acupuncture for Inflammation help?
Acupuncture stimulates your body to help your own body to make its own medicine, like giving your internal healing response a 10-20% boost. The pins spark your resources; what nature gave you and continues to give you.
Acupuncture and the other branches of Chinese medicine (nutrition, herbs, massage, heat therapy and exercise) restore homeostasis and keep the body functioning at an optimal level. When the body is functioning at an optimal level, we’re far less likely to get sick, and far more likely to recover quickly when we do get sick, inflammatory conditions included. Read more here about Traditional Chinese Medicine as a health modality here:
Autoimmune conditions are a chronic condition so healing is a longer process, the same way it took a long time for the autoimmune markers to show up in the first place. Never the less, we can balance your immune system with acupuncture and herbal medicine, dramatically help with nutrition specific for you as an individual and guide you to manage lifestyle factors to reduce autoimmune markers or better manage the symptoms.
If you think you may have inflammation happening in your body or have been diagnosed with an autoimmune condition, please contact us today to discuss how we can help you at our Acupuncture and Chinese Medicine clinic on the Sunshine Coast. Healing is possible. Being pain free, managing pain, feeling energetic, relaxing the stress response in the body and feeling an overall wellness is possible.
 Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
Links:
https://news.harvard.edu/gazette/story/2021/11/researchers-pinpoint-how-acupuncture-targets-inflammation/
https://pubmed.ncbi.nlm.nih.gov/24562381/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1781596/

by Tanya Keam | Jan 17, 2022 | Acupuncture, Chinese medicine, Client information, Frozen shoulder, Health practitioner, Muscle pain, Nambour, Shoulder pain, Sunshine coast, Uncategorized
Frozen shoulder Acupuncture and other treatment options
The shoulder can rotate in a full circle, unlike the elbow that only bends one way. Frozen shoulder is much like the name suggests. There is no movement or very limited movement in the shoulder capsule joint or the whole shoulder itself, it is frozen stuck. It can be quite painful as any slight attempt to move the shoulder joint or raise the arm, results in sever pain and restriction. If left untreated, it can lead a to a chronic condition. Below is further information of what causes it and frozen shoulder acupuncture treatment and other therapy options.
What is Frozen shoulder
Adhesive capsulitis (any word with the word ‘itis’ means inflammation) which is a shoulder condition that results in restriction and pain on range of motion. The muscles and tissues in your shoulder joint over time can become thicker and tighter leading to damage and scar tissue forming. As a result, the shoulder becomes restricted and extremely painful to move, to lay on and to even sleep.
What are the symptoms and stages of a Frozen shoulder
- The beginning stage is where the pain begins. We naturally try to avoid pain by reducing the arm movement and range of motion of the shoulder joint to stop the pain. Further inflammation and swelling can also result in reducing the amount of whole arm movement. Pain can feel dull, achy, sharp and worse on movement.
- The second stage is when the shoulder becomes frozen. Pain may even reduce however the joint becomes more difficult to move and is now stiff. For some people, the pain worsens at night, sometimes disrupting sleep.
- The last stage is when inflammation and swelling reduce in the shoulder capsule and the surrounding muscles, tendons and ligaments have more room to move more freely. Blood flow is also moving better so the range of motion beings to improve.
What can cause a Frozen shoulder
The bones, ligaments and tendons that make up your shoulder joint are encased in a capsule of connective tissue. Frozen shoulder occurs when this capsule thickens and tightens around the shoulder joint, restricting its movement (1).
It is sometimes not clear why this swelling occurs but can be linked to excessive use of the shoulder such as hyper-extending the joint, tearing of the tendons and muscles that support the shoulder structure or those who recently had to immobilise the shoulder for a long period, such as having it in a sling after surgery or an injury.
Frozen shoulder can be more common in:
- People 40 and older, particularly women
- People who’ve had prolonged immobility or reduced mobility of the shoulder
- People suffering from Diabetes, Parkinson’s disease, thyroid imbalance or cardiovascular disease
- People recovering from a stroke
What are some ways to help a frozen shoulder recover
- Decreasing pain first so a person can at least sleep properly to rest and recoup the body. Conventional medicine will offer use of anti-inflammatories and general pain relievers that offer temporary solutions. Steroid injections directly into the joint may be offered in some cases to attempt to reduce inflammation locally in the shoulder. There are some risks associated with traditional pain management.
- Increasing range of movement needs professional guidance so that the shoulder is not made worse or to push to the point of pain. If done incorrectly, pain and inflammation will cause further problems and restriction of movement – it may seize up. Exercises can be helpful to increase this range of movement.
- Acupuncture has been found in numerous research trials to have a strong impact and positive effect in pain reduction and improvement in shoulder mobility for frozen shoulder (2). Immediate and long lasting effects in the reduction of pain (3) is ideal as we want the shoulder to recover completely, not just have short term symptomatic relief that a pharmaceutical might provide.
- Mobilising the joint manually and massage therapy can help to loosen the tight muscles which improves movement and reduces pain. it is extremely important that this therapy is done gently so that too much pressure doest aggravate the condition.
- Surgery is usually considered as the last possible option after the above approaches have been applied, but may sometimes be necessary when the shoulder has damage to the muscle or tendons. Scans can be helpful to determine if surgery is even an option.
if you’re experiencing Frozen shoulder or other painful conditions, get in touch today to see if Acupuncture and other therapies used within our clinic may be of help to you. Contact Us or Book Online.
 Hi, I’m Tanya Keam,
Hi, I’m Tanya Keam,
an AHPRA registered Acupuncturist, bodyworker and doctor of Chinese medicine in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese and natural medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
References
- The mayo clinic: symptoms and causes: https://www.mayoclinic.org/diseases-conditions/frozen-shoulder/symptoms-causes/syc-20372684
- The Effectiveness of Acupuncture in the Treatment of Frozen Shoulder: A Systematic Review and Meta-Analysis, September 2020, Eyal Ben-Arie, Pei-Yu Kao, Wen-Chao Ho, Yu-Chen Lee, Evidence-based Complementary and Alternative Medicine2020(3):1-14.
- Immediate Pain Relief in Adhesive Capsulitis by Acupuncture: A Randomized Controlled Double-Blinded Study, Sven Schröder, MD, Dr. med. (PhD), Gesa Meyer-Hamme, MD, Thomas Friedemann, PhD, Sebastian Kirch, cand. med., Michael Hauck, MD, Dr. med. (PhD), Rosemarie Plaetke, PhD, Sunja Friedrichs, cand. med., Amit Gulati, PhD, Daniel Briem, MD, Dr. med. (PhD), Pain Medicine, Volume 18, Issue 11, November 2017.

by Tanya Keam | Sep 23, 2021 | Acupuncture, Chinese medicine, Client information, Health practitioner, Private health
Private Health for Acupuncture
Health Fund Changes Since 2019
Has there been private health fund changes?
There has been some changes to the private health insurance legislation. As of April 1, 2019 changes surrounding health fund rebates for complimentary therapies and natural medicine have commenced. You might be wondering if your favourite and preferred complimentary medicines have been excluded or not. The good news is, Private health for Acupuncture and Chinese medicine have not been affected by the change. They will continue to be listed under therapies with private health fund status.
Will I be able to claim benefits for Acupuncture from a qualified Chinese Medicine practitioner from my private health fund?
Yes! Acupuncture and Chinese Medicine have maintained their private health fund status. Depending on the type of private health insurance cover you have and are limited to, will determine how your health fund provider reimburses you. Tanya Keam would recommend you speak to your current health fund provider to ensure your current policy covers all that you need, such a hospital cover and the extras that you actually use. You may not need optical or dental as a extra for example. Your fund will ensure you have selected specific extras cover option that includes Acupuncture and Chinese Medicine.
What therapies HAVE BEEN affected by the changes?
The federal government has made a decision to no longer allow health fund providers to issue rebates for a number of natural therapies. These include:
- Alexander Technique
- Aromatherapy
- Bowen Therapy
- Buteyko Breathing technique
- Feldenkrais
- Homeopathy
- Iridology
- Kinesiology
- Naturopathy
- Pilates
- Reflexology
- Rolfing
- Shiatsu Massage
- Tai Chi
- Western Herbalism
- Yoga
How can I claim my private health insurance at Tanya Keam’s Clinic?
Tanya Keam’s Sunshine Coast Acupuncture Clinic has a health fund provider HICAPS terminal on site to facilitate your health fund transactions. You can then pay the gap amount via eftpos, credit card or cash – meaning you don’t need to follow up your rebate afterwards. You can find which health funds are available for on the spot claims here. Rare occasions when health funds or terminals are down, you will receive an invoice via email that you can send a PDF document straight to your health fund for reimbursement. How much you get back from your private health fund for Acupuncture and Chinese Medicine depends on your individual policy and the level of cover your health fund provides, such as a 50% rebate or a 20% rebate. Health funds will also be able to let you know what your limit is for the entirety of your policy year round, such as $400 or $1000 per year. Policies are usually a calendar year or financial year start date.
Patients often ask who is the best health fund to go with. That question is really something you and your family need to sit down and go over, depending on the level of cover you want and the premiums you want to pay to insure your health privately. Rebates can also only be obtained when you attend your booked appointment and your Acupuncturist has treated you. If for example you are sick or miss the appointment, the practitioner cannot issue you an invoice to claim despite the practitioners own treatment costs.
 If you have any further questions about private health rebates for your treatments then please contact us here or book online here.
If you have any further questions about private health rebates for your treatments then please contact us here or book online here.
Tanya Keam Wellness is a Chinese Medicine, Acupuncture and Natural Health Clinic in Nambour Heights, in the beautiful Sunshine Coast Hinterland in Queensland. Tanya welcomes her patients into the clinic with compassion and and open mind, while understanding their desired outcomes for current ailments and life-long optimal health. Her particular interest is in women’s health and fertility, pain, the immune system, mental health and preventative medicine. With continued training, Tanya works closely with patients from a integrative perspective by blending evidence-based healthcare with traditional eastern medicine.

by Tanya Keam | May 6, 2021 | Acupuncture, Adrenal Fatigue, Breast feeding, Chinese medicine, Client information, Hormones, Menstrual cycle, Nambour, Post Partum Depression, pregnancy, Sunshine coast, Wellness, Womens health
Post Partum Depression
Post Partum Depression includes feelings of deep sadness and emptiness accompanied by fatigue after childbirth. Low energy or even exhaustion after childbirth is completely common and normal that would last about a week. It isn’t just feeling drained after childbirth alone, carrying around all those extra kilograms for months is exhausting, especially if you’re working during pregnancy or you have other children to also look after. However if someone is feeling flat, anxious, crying a lot, experiencing panic attacks, feeling unconnected from their newborn for longer than 2 weeks, then this might be Post Partum Depression.
Symptoms associated with Post Partum Depression can include:
- Feeling overwhelmed, sad or hopeless
- Memory problems or trouble concentrating
- Feeling disconnected from the baby
- Loss of interest or pleasure in activities
- Crying a lot
- Broken sleep which leads to sleeping too little or too much
- Feeling withdrawn from family and friends
- Feeling worthless
- Having feelings of hurting yourself or the baby
- Racing thoughts
- Racing heart rate
- Having no energy or motivation
- Headaches, digestive complaints or other pains in the body
- No appetite
What causes Post Partum Depression?
Post Partum Depression isn’t completely understand but it thought the sudden drop in hormones; progesterone and oestrogen after childbirth has a significant role to play.
Estrogen and progesterone rise to the highest levels during pregnancy then suddenly plummet once the baby is born as the mother doesn’t need to keep feeding the baby via the placenta. The Thyroid gland that is involved with making hormones and regulating metabolism can also fluctuate or drop after childbirth leading to feelings of apathy and sadness.
How Common is Post Partum Depression?
More common than you think. Approximately 1 in 10 woman will experience some level of Post Partum Depression, with varying levels of severity and symptoms.
In very rare cases, Post Partum Psychosis may occur within the first 48-72 hours or up to the first 2 weeks after giving birth. It is considered an episode of bipolar illness with rapid periods or elation and feeling low, delusions or hallucinations.
What can you do to help yourself or a loved one who may be experiencing Post Partum Depression?
Get support. Untreated Post Partum Depression can lead to thoughts of self harm from the mother or further disconnection from the newborn where the mother feels like the baby is not hers. Contacting your doctor or paediatrician is the first step to get support.
Seeking further treatment from an allied health practitioner may also be helpful. Regulating the nervous system with Chinese medicine and Acupuncture, adjusting nutritional deficiencies and correcting hormonal imbalance with herbal medicine safe for breast feeding may be helpful.
Having a child is not easy, so getting the right support for the mother is the first step. You can book an appointment for our Sunshine Coast Acupuncture Clinic or give us a call to have a chat about your healthcare needs.
Phone: 0417 732 213
Further resources In Australia:
https://www.panda.org.au/

Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and integrative health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia.
I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
by Tanya Keam | Apr 6, 2021 | Acupuncture, Adrenal burnout, Adrenal Fatigue, Chinese medicine, Chronic fatigue, Client information, Daily Rituals, DIY Wellness Tips, fertility acupuncture, Health practitioner, Mental health, Nambour, Sunshine coast
What is Adrenal Fatigue?
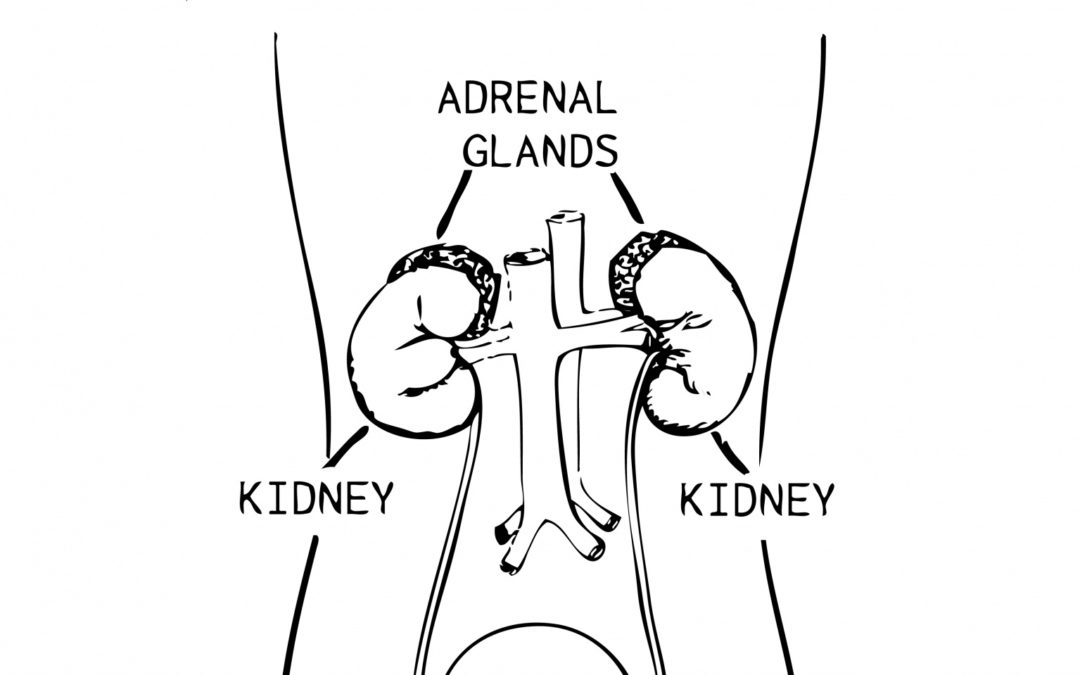
The Adrenal glands belong to the Endocrine System where they produce a variety of hormones that are essential to life. The medical term “Adrenal Insufficiency” is an inadequate production of one or more of these hormones as a result of underlying conditions. Whereas, Adrenal Fatigue isn’t an accepted medical diagnosis, it is thought that adrenal fatigue is caused by stress on the body where the adrenal glands cannot cope with the constant pace of fight-or-flight (sympathetic) nervous system response. adrenal fatigue acupuncture sunshine coast
tSigns and symptoms of adrenal insufficiency:
- Fatigue
- Body aches
- Unexplained weight loss
- Loss of body hair
- Skin discolouration
- Lightheadedness
- Low blood pressure
- Low production of hormones
Diagnosis for adrenal insufficiency can be tested to show inadequate levels of adrenal hormones.
In Traditional Chinese Medicine, adrenal fatigue is burnout. The kidney is the organ that stores our vital energy called Qi. We are all born with varying amounts of energy based on genetics, this is called out ancestral energy. This energy manages our reproduction, ageing, vitality and emotional-physical endurance. The day to day living of healthy food, exercise, relationships, environment and work/life balance is what maintains the kidney energy.
The less ancestral and vital kidney force you have (based on your lifestyle and if you’re over doing it), the sooner the chance of adrenal burnout. Chipping away at the kidney qi from too much stress, working too much without rest, living in the fight-or-flight (sympathetic) nervous system response WILL lead to adrenal burnout. When burn out is not addressed or the body is under continual strain over many years, there is a place that we cannot come back from. This leads to chronic health problems and the biggest symptom is long-term fatigue (exhaustion). The body is remarkable its in communication. Symptoms tell us something is wrong!
General fatigue can come and go, so having a holiday or some restful days off usually helps you to feel better naturally. Even having a blood test to check on a few things (such as iron levels) might be a simple explanation of fatigue. Adrenal fatigue however doesn’t just happen over night. It takes months or more of stress and over doing it to reach a point where the adrenal glands can’t keep going under pressure.
Traditional Chinese Medicine diagnoses adrenal fatigue based on multiple symptoms in relation to the energy of the kidney system. These can include :
- Fatigue and/or exhaustion
- Needing to sleep during the day after 8 hours of sleep at night
- Relying on coffee for energy
- Body aches
- Lower back pain
- Muscle weakness
- Lightheadness
- Shortness of breath
- Feel worse after exercise
- Loss of body hair or hair falling out
- Lack of concentration, focus or recall
- Low blood pressure
- Slow pulse rate
- Decreased libido
- Difficulty falling pregnant
- Thyroid imbalance
- Getting sick often or taking a long time to recover from illness
- Low blood sugar symptoms
- Waking early in the morning regularly at 4am
- Craving salty foods
- Emotional and mental instability such as anxiety
How does Traditional Chinese Medicine support someone with adrenal fatigue?
- Seeing a registered Acupuncturist allows you to receive the correct type of treatment based on their qualifications and experience. Adrenal fatigue acupuncture sunshine coast.
- Traditional acupuncture stimulates the internal healing response in the body to help the nervous system self regulate.
- Herbal medicine is prescribed based on the individual patient to support the energetics of the kidney and adrenal health.
- Moxibustion is a heat therapy used with acupuncture to further strengthen and support the bodies healing response.
- Correcting nutritional and mineral deficiencies to support optimal health.
- Lifestyle recommendations to support where the person is at. They may need a referral to a therapist to talk and gain some strategies to help cope with the demands that lead to adrenal burn out. Or something simple like gentle yoga exercises and breathing techniques to connect mind and body again. Life can get on top of you sometimes, so seeing a health practitioner, talking with someone close to you or a professional might be helpful.
What does rest look like?
- Sleep and naps during the day
- Time in nature
- Health treatments – having someone take care of you to rebalance your system
- Setting boundaries and changes to work-life balance
- Time off work
- Doing one thing at a time such as solely watching a movie, while you’re not on your phone or multitasking other things at the same time
- Laying down, putting your feet up with a book
- Time away from electronics and notifications from smart phones
- Asking for help
- Taking a holiday away from your regular environment
- Sitting down to eat, chew slowly, consciously taste and enjoy the food
- Gentle exercises to connect mind and body such as meditation, yoga, tai chi, qi gong, walks in nature all support the parasympathetic nervous system
To maintain the ancestral energy, we need to take care of ourselves with healthy food, exercise, quality sleep, managing stress and most importantly learning to rest.
If you are suffering from fatigue or you believe you may have adrenal fatigue please contact us today to discuss how we can help your adrenal fatigue at our Acupuncture clinic on the Sunshine Coast.
 Hi, I’m Tanya, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
Hi, I’m Tanya, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !

 Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Polycystic Ovarian Syndrome or Polycystic ovaries, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support your gynaecological health.
Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Polycystic Ovarian Syndrome or Polycystic ovaries, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support your gynaecological health.