by Tanya Keam | Jan 31, 2024 | Acupuncture, chinese herbal medicine, Chinese medicine, Client information, Fertility, Gynaecological, Menstrual cycle, PCOS, Period pain, PMS, Polycystic Ovarian Syndrome, pregnancy, Self care, Sunshine coast
Polycystic Ovarian Syndrome
Polycystic ovary syndrome (PCOS) is a hormonal problem that happens during the reproductive years. If you have PCOS, you may not have periods very often or your cycle is rarely a monthly cycle. Or you may have periods that last many days (1).
PCOS is classed as a hormonal and metabolic health imbalance affecting approximately 1 in 10 women. The male hormones androgens are higher in women with PCOS, as well as problems with insulin. Insulin is a peptide hormone secreted by cells of the pancreas to help maintain normal blood glucose levels, regulating carbohydrate, lipid and protein metabolism and promoting cell division and growth through its mitogenic effects (2). When insulin becomes resistant, that’s when disharmony with weight and hormonal changes can occur in women, thus having an impact on their reproduction.
What are the symptoms of Polycystic Ovarian syndrome?
- Irregular or no periods
- Excessive hair growth on the face or body
- Hair loss
- Skin conditions such as acne or excessive skin tags
- Difficulty falling pregnant due to irregular ovulation
- Difficulty losing weight and/or weight around the waist
- Mood changes and/or specifically anxiety or depression
Possible causes for Polycystic Ovarian syndrome
Genetics may play a role in PCOS, with up to a third of women having a female relative with PCOS or similar without being diagnosed. However lifestyle, diet and environmental factors show to be contributing factors also.
It is important to note that females can experience irregular periods without any of the other above symptoms. This is classed as polcystic ovaries (PCO); when you have multiple “cysts” on the ovaries. They aren’t actually cysts, they’re eggs that haven’t developed properly. It might occur after hormonal conceptive use in the reproductive years that confuse the body, and/or lifestyle or environmental factors. Insulin and weight are usually not of concern with PCO. The hypothalamic-pituitary-adrenal axis (HPA), describes the interaction between the hypothalamus, pituitary gland, and adrenal glands. The hypothalamus and pituitary gland are located just above the brainstem, while the adrenal glands are found on top of the kidneys (3). The HPA can receive the wrong signals resulting in eggs that haven’t developed properly (cysts), thus causing lack of ovulation and periods (4). Distinguishing between PCOS and PCO is important.
What can help Polycystic Ovarian syndrome?
PCOS treatment is mainly focussed on symptom management by reducing additional metabolic risk factors like heart disease and diabetes. Other ways can include:
- Regular exercise – managing potential weight gain and maintaining a healthy cardiovascular system
- Dietary changes – as PCOS has a somewhat inflammatory component, reducing inflammation via appropriate foods (a Mediterranean diet). Moderating carbohydrate intake in a similar way to balancing diabetes (insulin imbalances). Minimising exposure to foods that contain hormones that have been purposefully added to increase production – animal products usually.
- Acupuncture – can help with pain associated with PCOS and help regulate the nervous system which in turn has an impact on hormones
- Managing stress – stress impacts any health condition. Learning to manage life’s stressors is vital for general health and well being. Low stress also equals low cortisol release (the stress hormone). High cortisol leads to weight gain thus impacting the metabolic pathways exasperating PCOS
- Reducing exposure to hormone disrupting chemicals – did you know that IVF clinics do not allow perfumes/deodorants into their clinics as research has found that they can disrupt the endocrine system. In the armpit for example, products get directly absorbed into the lymphatic system. Going as natural as possible with skin care, body products and cleaning products will surely benefit
What does research say about Chinese medicine and Acupuncture for PCOS?
A study done in 2018 on the prevalence of diabetes mellitus, obesity, lipid metabolism disorders, and major depression was recorded as common symptoms for PCOS enrolled patients. Multiple common Chinese herbal formulas were included in the study based on the patients symptoms such as period pain, abdominal pain, constipation and uterine contractions.
The present findings revealed that patients with PCOS had a relatively high tendency to consult TCM practitioners (89.22%) due to Western medicine not having a treatment protocol directly. Among these prescription chinese herbal medicines (CHM) trialled showed hepatoprotective effects, as well as beneficial effects in treatment of hyperglycemia, insulin intolerance, dyslipidemia, and anovulation. These findings indicate that Chinese herbal medicine might serve as a potentially effective therapeutic option for PCOS (5).
Another study showed that following transfer of fresh or frozen-thawed embryos available from the same stimulated IVF cycle, 47 patients got clinical pregnant and 43 of them achieved live birth with the use of CHM. Among which, 32 patients achieved term delivery in the CHM group. In the non-CHM group, 27 patients got clinical pregnant and 22 of them achieved live birth, among which, 14 patients achieved term delivery (6).
The NHMRC Centre for Research Excellence in PCOS undertaken at the Sydney Western University, has already completed a systematic review, and a qualitative study on acupuncture for weight loss in PCOS, with feasibility testing now in sight for a clinical trial. The clinical trial will explore the role of traditional acupuncture as an adjunct to lifestyle interventions for weight loss in PCOS. “Weight loss improves many of the features of PCOS and can reduce the burden of chronic disease from diabetes and heart disease.” (7).
 Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Polycystic Ovarian Syndrome or Polycystic ovaries, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support your gynaecological health.
Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Polycystic Ovarian Syndrome or Polycystic ovaries, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support your gynaecological health.
You can see Tanya’s training here, call us here, or book online here.
References:
- https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
- Wilcox. G. 2005. Insulin and Insulin resistance. National Library of medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1204764/
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009 Jul;5(7):374-81. doi: 10.1038/nrendo.2009.106. Epub 2009 Jun 2. PMID: 19488073. https://neuroscientificallychallenged.com/posts/what-is-the-hpa-axis
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009 Jul;5(7):374-81. doi: 10.1038/nrendo.2009.106. Epub 2009 Jun 2. PMID: 19488073. https://neuroscientificallychallenged.com/posts/what-is-the-hpa-axis
- Liao, Wan-ting, Chiang. Jen-huai, Li Chia-lung, Lee Ling-Tsung, Su Cheng-chiung, Yen Hung-rong. 2018 J Clin Med. 2018 Jul; 7(7): 179. Journal of Clinical Medicine. Investigation on the Use of Traditional Chinese Medicine for Polycystic Ovary Syndrome in a Nationwide Prescription Database in Taiwan. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6069244/
- 6. P, Xiaoming. Gu, Yinger. Z Xian. W, Fangfang. S, Biwei. C, Long. W, fangfang. Q, fan. Integrative Medicine research Volume 11, Issue 1, March 2022, 1007752022. Chinese herbal medicine (Bu-Shen-Tian-Jing Formula) for outcomes of IVF in Chinese patients with polycystic ovary syndrome: A retrospective cohort study. https://www.sciencedirect.com/science/article/pii/S2213422021000627
- NICM Health Research Institute: https://westernsydney.edu.au/nicmhri/news/trial_to_explore_acupuncture_for_weight_loss_in_pcos

by Tanya Keam | Jan 10, 2024 | Acupuncture, Bloating, Chinese medicine, Client information, Emotions, fertility acupuncture, Gynaecological, Herbal remedies, Hormones, Menstrual cycle, Nambour, Period pain, PMS, Premenstrual Dysmorphic Disorder, Self care, Stress, Sunshine coast, Womens health
Chinese Medicine for Premenstrual Dysmorphic Disorder
Premenstrual Dysmorphic Disorder (PMDD) is a health concern that is similar to premenstrual syndrome (PMS) but is more serious. PMDD causes severe moodiness such as feeling irritable, crying a lot, depression, anger outbursts or anxiety in the week or two before the period starts. Other symptoms may include fatigue, weight gain, restless sleep, breast tenderness, digestion changes, trouble focussing, binge eating, feeling out of control and suicidal thoughts.
About 80% of women report at least mild premenstrual symptoms, 20%–50% report moderate-to-severe premenstrual symptoms, and about 5% report severe symptoms for several days with impairment of functioning. The 5% of women with the severest premenstrual symptoms and impairment of social and role functioning often meet the diagnostic criteria for premenstrual dysphoric disorder (PMDD) (1).
Risk factors may include:
- A family history of PMS or PMDD
- Women with a personal or family history of depression, postpartum depression, or other mood disorders
- Cigarette smoking (2)
How is PMDD diagnosed?
Premenstrual Dysmorphic Disorder (PMDD) is typically diagnosed by a healthcare provider after performing a physical examination and speaking to the patient about signs and symptoms. Researchers do not know for sure what causes PMDD or PMS, however hormonal changes in the menstrual cycle each month may play a role due to the brain chemical called serotonin levels changing throughout the cycle.
Healthcare providers may also ask patients to keep track of symptoms over several menstrual cycles, or order tests to check certain things related to hormones.
What are the treatment options for PMDD?
Treatment for Premenstrual Dysmorphic Disorder (PMDD) typically involves a combination of lifestyle changes and medications. Medications used to treat PMDD include antidepressants, hormonal control pills/medications, or non-steroidal anti-inflammatory drugs. In some instances, gonadotropin releasing hormones may be given.
Natural approaches for Premenstrual Dysmorphic Disorder (PMDD) can include regular exercise and nutritional changes individualised to the patient to support serotonin, and lifestyle modifications such as sticking to a daily routine, practicing meditation and taking care of oneself, recognising emotions and managing stressful situations. Other natural remedies that have been used to treat symptoms associated with PMDD include acupuncture and herbal medicine.. Traditional Chinese medicinal herbs can be given to patients the week or two before their period is due to ease symptoms. This can be a good alternative to pharmaceuticals.
It’s important to remember than it’s normal for women and young girls to experience fluctuations in energy levels, mood or food cravings in different stages of their menstrual cycle. Iron levels for example drop once the uterus lining has shed, so it’s normal to feel lower energy before or on your period. Women live on a 28 day cycle and can sometimes even sync with the moon cycles. Whereas, men live on a 24 hour one! However when signs and symptoms are really affecting your quality of life, then it’s important to seek help.
 Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Chinese Medicine Premenstrual Dysmorphic Disorder treatment specifically, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support you to feel better.
Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Chinese Medicine Premenstrual Dysmorphic Disorder treatment specifically, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support you to feel better.
You can see Tanya’s training here, call us here, or book online here.
References:
- Pearlstein, T., Steiner, M. (2008). Premenstrual dysphoric disorder: burden of illness and treatment update. Journal of Psychiatry & Neuroscience; 33(4): 291–301.
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/premenstrual-dysphoric-disorder-pmdd
by Tanya Keam | Jan 6, 2020 | Acupuncture, Chinese medicine, Client information, Endometriosis, Fertility acupucnture, Gynaecological, Pain, Period pain, pregnancy, Stress, Sunshine coast, Womens health, Yin
Endometriosis and Chinese Medicine
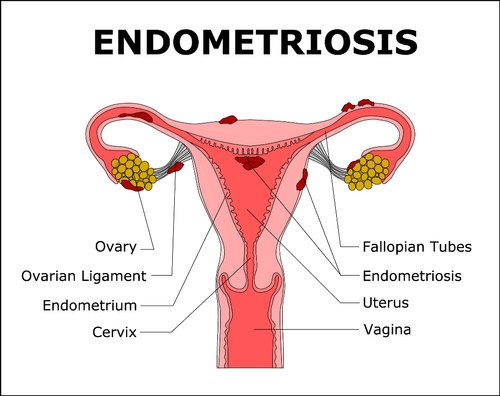
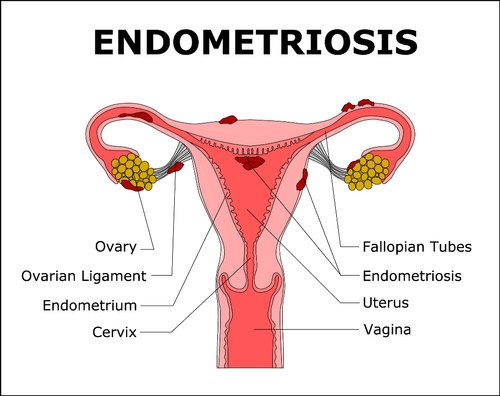
First of all, What is Endometriosis? Endometriosis is a common condition in which the tissue that is similar to the lining of the womb grows outside of the uterus and in other parts of the pelvic cavity. Whilst endometriosis most often affects the reproductive organs, thus damaging fertility, it is also frequently found in the bowel and bladder, but has rarely been found in muscle, joints, the lungs and the brain. More than 10% of Australian women suffer from Endometriosis at some point in their life (1). Endometriosis and Chinese medicine
Some women experience Endometriosis as debilitating period pain, pelvic pain and pain during intercourse. They may need to seek medical attention to ease their painful symptoms. While others have no symptoms but may have difficult falling pregnant naturally (1, 2).
How is Endometriosis diagnosed?
Patients will generally have a pelvic examination and internal and external ultrasounds first to look at the whole lower pelvis including ovaries, fallopian tubes and uterus, however Laparoscopy (key hole surgery) is needed to confirm diagnosis.
There are multiple stages of Endometriosis Endometriosis and Chinese medicine
- Mild Endometriosis appears in small patches or surface lesions scattered around the pelvic cavity.
- Moderate Endometriosis appears as larger widespread starting to infiltrate tissue and often found on the ovaries, pouch of douglas and utero-sacral ligaments.
- Severe Endometriosis affects most of the pelvic organs, often with distortion of the anatomy and the adhesions (1).
What can cause of Endometriosis?
- In utero exposure to a non-steriodal oestrogen that was commonly given to woman (prior to 1971) as it was thought to reduce the risk of pregnancy complications
- Use of low dose contraceptives
- A family history (first generation) can make you more prone to having Endometriosis
- Irregular menstrual cycles that are heavy and prolonged
- Delayed childbearing
- Teenagers starting their period after the age of 15 years
- A high amount of physical exercise from a low teenage years
- Multiple births and prolonged lactation
- Hormonal defects such as Mullein duct defects
Conventional Treatment Options
- Your doctor typically recommends trying conservative treatment approaches first, depending on how severe your signs and symptoms are and whether you hope to become pregnant. If this fails then surgery is the next option.
- Over the counter pain medicines such as NSAIDS.
- Hormone therapy to slow endometrial tissue growth and prevent new implants of endometrial tissue. Hormone therapy is only temporary as they are suppressing hormones, so once treatment stops, your symptoms may return.
- Hormonal contraceptives – the birth control pill, vaginal rings or patches. Many women have lighter and shorter menstrual flow when they’re using a hormonal contraceptive.
- Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists – These drugs block the production of ovarian-stimulating hormones, lowering estrogen levels and preventing menstruation. This causes endometrial tissue to shrink.
- Aromatase inhibitors – a class of medicines that reduce the amount of estrogen in your body.
- Progestin therapy – a variety of progestin therapies, including an intrauterine device with levonorgestrel (Mirena, Skyla), contraceptive implant (Nexplanon), contraceptive injection (Depo-Provera) or progestin pill (Camila), can halt menstrual periods and the growth of endometrial implants, which may relieve endometriosis signs and symptoms.
- Laproscopy surgery to help remove a lot of the endometrial tissue, while trying to preserve the ovaries and uterus. This is helpful if you doctors plan is to improve chances of conceiving and your diagnosis is in the severe.
- Hysterectomy – surgical removal of the uterus and cervis and sometimes the fallopian tubes and ovaries. This type of treatment is the last resort and should only be considered when the woman has already conceived children and is of age that is suitable (3).
Endometriosis and Chinese Medicine
Endometriosis is seen as a ‘blood stagnation’ pattern. When the Endometrial tissue is outside of the uterus, it forms a blockage preventing blood from exiting downward out of a woman’s body, instead it pools in the pelvic cavity which therefore causes severe pain.
The treatment of Endometriosis with Chinese medicine has a specific emphasis on looking at the whole menstrual cycle and promoting proper circulation of blood through each week of the cycle. Promoting blood flow in this way reduces pain during menstruation, reduces and prevents the endometrial tissue that builds up in the pelvic cavity and decreased inflammation, thus restoring a healthy and functioning reproductive system.
In the traditiol of Chinese medicine, different areas and prescription are used for each individual such as acupuncture treatment, moxibustion (heat therapy). herbal medicines such as Peony Root (4) that is often used for menstrual disorders, nutritional and lifestyle advice.
Advice from Endometriosis Australia
Using other health professionals such as physiotherapists, acupuncturists, herbalists, nutritionists, homeopaths and psychologists can be very helpful for women with endometriosis. You should discuss these treatments with your doctor before commencing them, or if you are on any of these treatments and are having surgery, then it is also important to tell your doctor.
Research:
- Endometriosis Australia > https://www.endometriosisaustralia.org
- Lyttleton, J. & Clavey, S. (2004). Treatment of Infertility with Chinese Medicine. UK. Elsevier.
- Endometriosis 2018. Mayo Clinic > https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- Takeuchi, T. Nishii, O. Okamura, T et al. Effect of Paeoniflorin, Glycyrrhizin and Glycyrrhetic acid on Ovarian Androgen Production, The American Journal of Chinese Medicine, 19(1), 1991, pp73-8) > https://www.worldscientific.com/doi/pdf/10.1142/S0192415X91000119
- Briden, L. 2018. Period Repair Manual: Every Woman’s Guide to Better Periods. Pan Macmillan Australia Pty Ltd, NSW, Australia.
If you are ready to seek support from an experienced health professional in women’s health for Endometriosis with Chinese medicine and Acupuncture, you can book an appointment for our Sunshine Coast Clinic or give us a call if you have further questions.
Phone: 0417 732 213
 Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and integrative health professional in Nambour on the beautiful Sunshine Coast, Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living.
Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and integrative health professional in Nambour on the beautiful Sunshine Coast, Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living.
 Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Polycystic Ovarian Syndrome or Polycystic ovaries, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support your gynaecological health.
Tanya Keam is an integrative Chinese medicine Doctor and registered Acupuncturist in Nambour in the beautiful Sunshine Coast hinterland in Queensland, Australia. If you’re experiencing the above symptoms or interested in Traditional Chinese Medicine and Acupuncture treatment specifically for Polycystic Ovarian Syndrome or Polycystic ovaries, please reach out to see if Acupuncture, herbal medicine and lifestyle guidance might support your gynaecological health.