by Tanya Keam | Aug 30, 2022 | Acupuncture, Autoimmune, Chinese medicine, Client information, Exercise, Immune Support, Immune system, Inflammation, Joint pain, Nambour, Nutrition, Pain, Stress, Sunshine coast
Acupuncture for Inflammation is showing positive results in research. Inflammation refers to your body’s process of fighting against things that harm it, like infections, injuries, and toxins, in an attempt to heal itself. When something damages the cells, your body releases chemicals that trigger a response from your immune system.
Chronic inflammation can cause autoimmune disorders, such as Lupus or Chron’s, where your body attacks healthy tissue. Exposure to toxins, like pollution or industrial chemicals. Untreated acute inflammation, such as from an infection or injury.
Other factors that contribute significantly to inflammation is poor diet and stress.
What about stress?
- Working too much, over doing it
- Poor diet
- Lack of exercise
- Environmental factors
- Emotional distress
- Not taking care of yourself
- Injury, trauma – sometimes inflammation is a good thing when there’s been trauma to the body. However its important to quickly reduce the inflammation so the body can heal and get well
Try to avoid these “foods” when grocery shopping:
- Refined carbohydrates, such as white bread and pastries
- Hot chips and other fried foods (often fried in canola oil which is GMO)
- Margarine
- Soft drinks and other sugar-sweetened beverages (including some alcoholic drinks)
- Red meat and processed meat (hot dogs, sausages)
- Corn syrup
- Packaged foods with ingredient and numbers on the ingredients list you don’t understand
- Drive-through foods
Other foods that may contribute to inflammation in the body for some people may include:
- Gluten (proteins trigger the immune system to jump into action, causing inflammation). This inflammation can affect the body’s organs and soft tissue. However sometimes, its the pesticides, herbicides or other chemicals used in the processing of certain grains which can cause gluten sensitivity.
- Dairy
- Soy
- Corn
- White sugar
An anti-inflammatory diet is rich in good oils, fats, omega’s and antioxidants…
- Olive oil, flaxseed oil
- Green leafy vegetables (such as spinach, kale, and collards)
- Nuts
- Tumeric, ginger
- Fatty fish (like salmon, mackerel, tuna and sardines)
- Fruits (such as avocado, strawberries, blueberries, cherries, goji berries, pineapple, papaya)
- Raw unprocessed honey
- Coconut
- Tomato
- Bone broth
- Ghee
- A rainbow of fruits and vegetables
Try to eat as organic and local as possible. In season fruits and vegetables are also important. Certified organic can be expensive so if you cant source it, make sure you thoroughly wash your food. Or better yet start a little vegie garden and grow what you can at home.
How can Chinese medicines and Acupuncture for Inflammation help?
Acupuncture stimulates your body to help your own body to make its own medicine, like giving your internal healing response a 10-20% boost. The pins spark your resources; what nature gave you and continues to give you.
Acupuncture and the other branches of Chinese medicine (nutrition, herbs, massage, heat therapy and exercise) restore homeostasis and keep the body functioning at an optimal level. When the body is functioning at an optimal level, we’re far less likely to get sick, and far more likely to recover quickly when we do get sick, inflammatory conditions included. Read more here about Traditional Chinese Medicine as a health modality here:
Autoimmune conditions are a chronic condition so healing is a longer process, the same way it took a long time for the autoimmune markers to show up in the first place. Never the less, we can balance your immune system with acupuncture and herbal medicine, dramatically help with nutrition specific for you as an individual and guide you to manage lifestyle factors to reduce autoimmune markers or better manage the symptoms.
If you think you may have inflammation happening in your body or have been diagnosed with an autoimmune condition, please contact us today to discuss how we can help you at our Acupuncture and Chinese Medicine clinic on the Sunshine Coast. Healing is possible. Being pain free, managing pain, feeling energetic, relaxing the stress response in the body and feeling an overall wellness is possible.
 Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
Links:
https://news.harvard.edu/gazette/story/2021/11/researchers-pinpoint-how-acupuncture-targets-inflammation/
https://pubmed.ncbi.nlm.nih.gov/24562381/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1781596/
by Tanya Keam | Jan 6, 2020 | Acupuncture, Chinese medicine, Client information, Endometriosis, Fertility acupucnture, Gynaecological, Pain, Period pain, pregnancy, Stress, Sunshine coast, Womens health, Yin
Endometriosis and Chinese Medicine
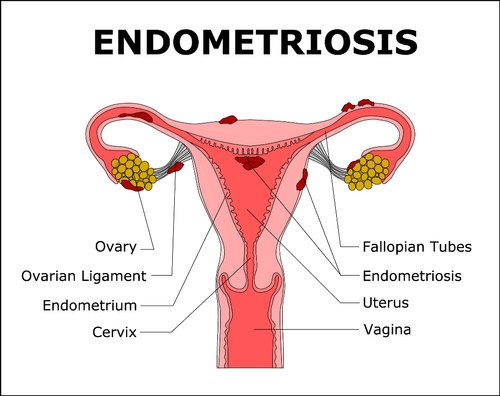
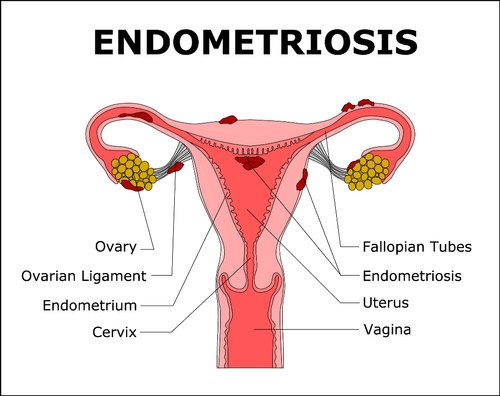
First of all, What is Endometriosis? Endometriosis is a common condition in which the tissue that is similar to the lining of the womb grows outside of the uterus and in other parts of the pelvic cavity. Whilst endometriosis most often affects the reproductive organs, thus damaging fertility, it is also frequently found in the bowel and bladder, but has rarely been found in muscle, joints, the lungs and the brain. More than 10% of Australian women suffer from Endometriosis at some point in their life (1). Endometriosis and Chinese medicine
Some women experience Endometriosis as debilitating period pain, pelvic pain and pain during intercourse. They may need to seek medical attention to ease their painful symptoms. While others have no symptoms but may have difficult falling pregnant naturally (1, 2).
How is Endometriosis diagnosed?
Patients will generally have a pelvic examination and internal and external ultrasounds first to look at the whole lower pelvis including ovaries, fallopian tubes and uterus, however Laparoscopy (key hole surgery) is needed to confirm diagnosis.
There are multiple stages of Endometriosis Endometriosis and Chinese medicine
- Mild Endometriosis appears in small patches or surface lesions scattered around the pelvic cavity.
- Moderate Endometriosis appears as larger widespread starting to infiltrate tissue and often found on the ovaries, pouch of douglas and utero-sacral ligaments.
- Severe Endometriosis affects most of the pelvic organs, often with distortion of the anatomy and the adhesions (1).
What can cause of Endometriosis?
- In utero exposure to a non-steriodal oestrogen that was commonly given to woman (prior to 1971) as it was thought to reduce the risk of pregnancy complications
- Use of low dose contraceptives
- A family history (first generation) can make you more prone to having Endometriosis
- Irregular menstrual cycles that are heavy and prolonged
- Delayed childbearing
- Teenagers starting their period after the age of 15 years
- A high amount of physical exercise from a low teenage years
- Multiple births and prolonged lactation
- Hormonal defects such as Mullein duct defects
Conventional Treatment Options
- Your doctor typically recommends trying conservative treatment approaches first, depending on how severe your signs and symptoms are and whether you hope to become pregnant. If this fails then surgery is the next option.
- Over the counter pain medicines such as NSAIDS.
- Hormone therapy to slow endometrial tissue growth and prevent new implants of endometrial tissue. Hormone therapy is only temporary as they are suppressing hormones, so once treatment stops, your symptoms may return.
- Hormonal contraceptives – the birth control pill, vaginal rings or patches. Many women have lighter and shorter menstrual flow when they’re using a hormonal contraceptive.
- Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists – These drugs block the production of ovarian-stimulating hormones, lowering estrogen levels and preventing menstruation. This causes endometrial tissue to shrink.
- Aromatase inhibitors – a class of medicines that reduce the amount of estrogen in your body.
- Progestin therapy – a variety of progestin therapies, including an intrauterine device with levonorgestrel (Mirena, Skyla), contraceptive implant (Nexplanon), contraceptive injection (Depo-Provera) or progestin pill (Camila), can halt menstrual periods and the growth of endometrial implants, which may relieve endometriosis signs and symptoms.
- Laproscopy surgery to help remove a lot of the endometrial tissue, while trying to preserve the ovaries and uterus. This is helpful if you doctors plan is to improve chances of conceiving and your diagnosis is in the severe.
- Hysterectomy – surgical removal of the uterus and cervis and sometimes the fallopian tubes and ovaries. This type of treatment is the last resort and should only be considered when the woman has already conceived children and is of age that is suitable (3).
Endometriosis and Chinese Medicine
Endometriosis is seen as a ‘blood stagnation’ pattern. When the Endometrial tissue is outside of the uterus, it forms a blockage preventing blood from exiting downward out of a woman’s body, instead it pools in the pelvic cavity which therefore causes severe pain.
The treatment of Endometriosis with Chinese medicine has a specific emphasis on looking at the whole menstrual cycle and promoting proper circulation of blood through each week of the cycle. Promoting blood flow in this way reduces pain during menstruation, reduces and prevents the endometrial tissue that builds up in the pelvic cavity and decreased inflammation, thus restoring a healthy and functioning reproductive system.
In the traditiol of Chinese medicine, different areas and prescription are used for each individual such as acupuncture treatment, moxibustion (heat therapy). herbal medicines such as Peony Root (4) that is often used for menstrual disorders, nutritional and lifestyle advice.
Advice from Endometriosis Australia
Using other health professionals such as physiotherapists, acupuncturists, herbalists, nutritionists, homeopaths and psychologists can be very helpful for women with endometriosis. You should discuss these treatments with your doctor before commencing them, or if you are on any of these treatments and are having surgery, then it is also important to tell your doctor.
Research:
- Endometriosis Australia > https://www.endometriosisaustralia.org
- Lyttleton, J. & Clavey, S. (2004). Treatment of Infertility with Chinese Medicine. UK. Elsevier.
- Endometriosis 2018. Mayo Clinic > https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- Takeuchi, T. Nishii, O. Okamura, T et al. Effect of Paeoniflorin, Glycyrrhizin and Glycyrrhetic acid on Ovarian Androgen Production, The American Journal of Chinese Medicine, 19(1), 1991, pp73-8) > https://www.worldscientific.com/doi/pdf/10.1142/S0192415X91000119
- Briden, L. 2018. Period Repair Manual: Every Woman’s Guide to Better Periods. Pan Macmillan Australia Pty Ltd, NSW, Australia.
If you are ready to seek support from an experienced health professional in women’s health for Endometriosis with Chinese medicine and Acupuncture, you can book an appointment for our Sunshine Coast Clinic or give us a call if you have further questions.
Phone: 0417 732 213
 Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and integrative health professional in Nambour on the beautiful Sunshine Coast, Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living.
Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and integrative health professional in Nambour on the beautiful Sunshine Coast, Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living.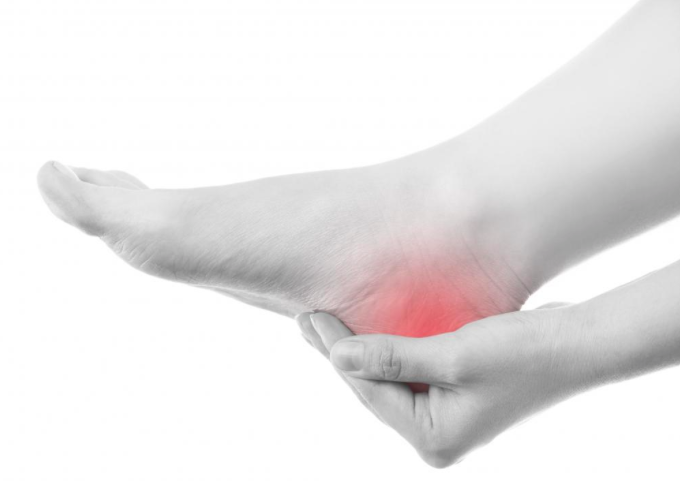
by Tanya Keam | Nov 1, 2019 | Acupuncture, Chinese medicine, Client information, Exercise, Health practitioner, Heel pain, Joint pain, Muscle pain, Nambour, Pain, Plantar Fasciitis, Sunshine coast
Acupuncture for Plantar Fasciitis
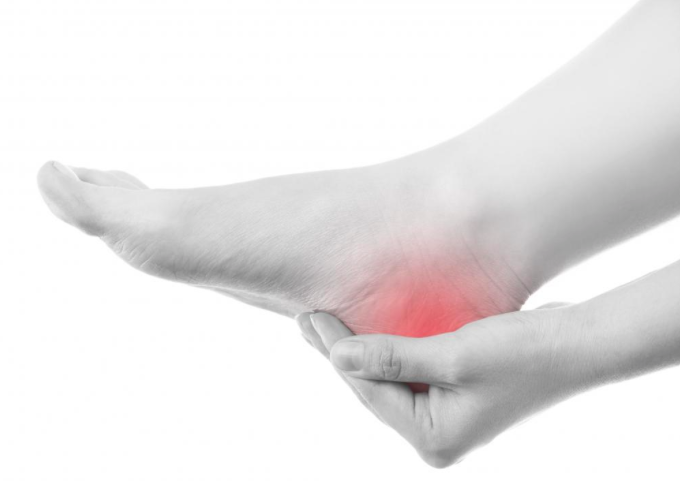
Imagine crawling out of bed, half asleep and feeling the pain of standing on a nail or a hot amber right in your heel. You crumble, knees buckle, jaw clenched in pain … this is Plantar Fasciitis! Acupuncture for Plantar Fasciitis.
What is Plantar Fasciitis?
The plantar fascia is a piece of strong and thick tissue that runs along the bottom of the foot. It connects the heel bone to the toes, creating the foot’s arch. Plantar fasciitis is inflammation of the plantar fascia.
It can be caused by:
- Playing certain sports that put stress on the heel bone or recent increased activity
- Flat-footed, high arches or collapsing arches
- Being overweight
- Pregnancy
- Muscle tension in the legs
- Standing for long periods
- Standing on hard surfaces
- Heel spur
- Injury
- Wearing incorrect shoes
- Misalignment of the pelvis or hips
Based on an Australian local population study of 3206 participants, the prevalence of heel pain was 3.6% (1).
What are the symptoms of Plantar Fasciitis?
Pain! Which tends to be aggravated by:
- Long periods of standing or sitting
- When you first step out of bed in the morning and place your feet on the ground
- After increased physical activity in the lower half the body
How do you know if you could be experiencing Plantar Fasciitis?
Because pain is the main debilitating symptom, in most cases diagnosis is by the presenting symptoms and location of pain in the heel. The achilles tendon is also examined for inflammation. Further investigations such as ultrasound or X-ray may be used to rule out other conditions.
How is Plantar Fasciitis treated?
- Pain relief medications
- Steriod injections into the heel
- Activity adjustments or rest
- Appropriate stretching
- Acupuncture therapy
- Massage therapy
- Sole inserts for shoes
- Change in footwear or padding when standing for long periods
- Rest
- Nutritional adjustments
The most effective treatment plan for Plantar Fasciitis is to first remove the cause, then apply stretching and treatment which results in resolving inflammation and pain.
Chinese medicine views of Plantar Fasciitis
Predominantly with the view that there is a stagnation in the flow of Blood and Qi in the affected are, this may also be accompanied by heat in the local area (inflammation). For this condition, a combination of Chinese Medicine practices may be used.
How can Chinese medicine help?
Firstly, figure out the cause, then apply the correct treatment.
Structural alignment of the body – Assessing whether your pelvis/hips or spine is out of alignment determines whether your feet are hitting the ground correctly.
Diet – Modern understanding of gut health has shown poor gut function can significantly increase inflammation in the body. Looking into your nutrition and your eating habits may assist overall health and therefore provide pain relief for issues such as Plantar Fasciitis and also prevent inflammation.
Nutritional supplementation – Foods and herbs can be useful for reducing inflammation. Such as Omega’s, Tumeric and Magnesium.
Acupuncture – Trials have showed potential positive effects in the treatment for Plantar Fasciitis. Acupuncture can be effective at reducing muscle tension and as such can help to reduce the pressure and strain on the fascia in Plantar Fasciitis. Electro-acupuncture coupled with conventional treatments (stretching exercises, shoe modification and analgesics) provided a success rate of 80% in chronic Planar Fasciitis which was more effective than conventional treatments alone (2). Future research should recognise the complexity of plantar heel pain, of acupuncture and of the relationship between them, to explore the optimum use and integration of this approach (3).
Other techniques – massage, cupping, gua sha, liniments to accompany acupuncture.
Lifestyle recommendations – Adjustment of posture, specified stretches, appropriate footwear and prevention about contributing factors that may be aggravating the condition.
If you are suffering from plantar fasciitis or believe you may have something similar such as burning heel pain please contact us today to discuss how we can help you at our Sunshine Coast Acupuncture clinic with your plantar fasciitis or other pain conditions.
 Hi, I’m Tanya, an Acupuncturist and health practitioner in Nambour on the Sunshine Coast, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
Hi, I’m Tanya, an Acupuncturist and health practitioner in Nambour on the Sunshine Coast, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
References:
- Source- Allan J Pollack, Helena Britt (2015) Plantar fasciitis in Australian general practice Volume 44, No.3, 2015 Pages 90-91, Retrieved from https://www.racgp.org.au/afp/2015/march/plantar-fasciitis-in-australian-general-practice/
- The American Journal of Chinese Medicine, An International Journal of Comparative Medicine East and West. Efficacy of Electro-Acupuncture in Chronic Plantar Fasciitis: A Randomized Controlled Trial. Wipoo Kumnerddee and Nitsara Pattapong. Issue 06, Volume 40, 2012. Retrieved from https://www.worldscientific.com/doi/abs/10.1142/S0192415X12500863
- Clark Richard J, Tighes Maria, The Effectiveness of Acupuncture for Plantar Heel Pain: a systematic review. Acupuncture in Medicine. October 2012. Retrieved from https://journals.sagepub.com/doi/abs/10.1136/acupmed-2012-010183https://journals.sagepub.com/doi/abs/10.1136/acupmed-2012-010183

 Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !
Hi, I’m Tanya Keam, an AHPRA registered Acupuncturist and health practitioner in Nambour in the Sunshine Coast hinterland, Queensland Australia. I practice Chinese medicine because its safe, logical, relevant and has effectively shown methods of natural wellness for thousands of years (read more about my training here). Life doesn’t need to be complicated and nor does the treatment approaches to get people feeling vibrant and well. I’ve seen people gain a lot from treatments, much more than just alleviating symptoms. It’s exciting to connect with people and share deep wisdom from the classics of ancient and traditional medicine, with modern protocols for todays mind-body living. See you in the clinic !